Intraoperative Neurophysiology?
The first question asked by everyone when they hear of intraoperative neurophysiology is… what is it?
Intraoperative neurophysiology is a discipline of clinical neuroscience that is used in the operating theatres of orthopaedics and neurosurgery that helps monitor the real time function of the human nervous system.
During brain, brainstem, spinal cord and vascular procedures, there is risk of damage to neurological structures may impede our ability to feel, hear, speak, move and touch. Therefore neurophysiology is employed in real time during surgery to help identify, and monitor the functional status of these critical structures, to ensure optimal post-operative outcomes.
This type of monitoring is performed by Neurophysiology Scientists, who are highly trained neuroscientists that use a sensitive array of electrodes to stimulate and record electrical activity from muscles and nerves, and communicate with the surgical team to provide real time information during the surgical procedure.
Monitoring Modalities
There are a great number of clinical tests that we can perform routinely during procedure to evaluate neurological function, which we call ‘modalities’. These tests are often performed in conjunction with one another in a ‘multi-modal’ monitoring approach which is considered gold standard to provide a complete understanding of the patients nervous system. Here is a list of modalities commonly employed by Praxis;
Transcranial Motor Evoked Potentials
Electromyography
Direct Nerve Stimulation
Triggered Electromyography
Somatosensory Evoked Potentials
Corticobulbar Motor Evoked Potentials
Facial Nerve EMG
Auditory Evoked Potentials
Cranial Nerve EMG - CN III-XII
Blink Reflex
Laryngeal Nerve Monitoring
Compound Nerve Action Potentials
D-Wave Monitoring
Dorsal Column Mapping
Direct Cortical Stimulation for Motor Mapping
Transcranial Motor Evoked Potentials
Transcranial Motor Evoked Potentials ‘TcMEPs’ are a major workhorse of intraoperative neurophysiological technique, that monitors the voluntary motor functions of the arms, trunk and legs. This test is used in majority of spinal procedures to ensure function of the spinal cord and corticospinal tract is maintained.
This test works by stimulating the primary motor cortex in the brain using electrodes placed on the scalp, that depolarise the neurons in the corticospinal tract, which descend the brainstem and spinal cord, exit the spinal canal, and innervate our muscles. Using needle electrodes placed into the muscles we can then record the evoked response to evaluate amplitude and latency. By repeating this test regularly during surgical manoeuvres we can keep an eye on motor function.
Electromyography
Electromyography, ‘EMG’ is another staple of monitoring employed in many procedures. Like TcMEP’s it involves the recording of electrical activity from the muscles, however unlike TcMEPs, the activity recorded is spontaneous in nature and able to record activity generated by surgical manipulations. The data recorded can inform surgeons about the status of peripheral nerve roots and prevent unwanted damage. This feedback can prompt swift surgical intervention and prevent any unwanted complications.
Direct Nerve Stimulation / triggered Electromyography
Direct Nerve Stimulation (DNS) or triggered EMG is a technique again similar to TcMEPs and EMG, whereby using needles electrodes placed in target muscles, we can infer functional status of the muscles innervating nerve root. DNS/tEMG can be used in a variety of scenarios; such as pedicle screw integrity testing, nerve root identification, and for safe traversal of the psoas during lateral lumbar interbody fusion.
During pedicle screw insertions, it is possible to stimulate the screw to evaluate its placement in bone, should an implant breach the bone, stimulation can innervate nerves and provide early warning that the trajectory of a pedicle screw is close to nerves. Similarly, during procedures that operate close to peripheral nerves, it is possible to stimulate these nerves to provide functional identification and evaluation. This is useful during resection of lesions where neural elements are displaced and need to be located. During lateral fusion surgery of the lumbar spine, traversing the psoas poses a threat to the lumbrosacral plexus which descends alongside the muscle. By using DNS/tEMG we can evaluate the proximity to nerves to avoid damage during the approaches retraction.
Somatosensory Evoked Potentials
Somatosensory Evoked Potentials (SSEP), is a widely used technique during many procedures and looks to evaluate the ascending sensory function. Where motor function travels down the anterior, and anterior-lateral portions of the spinal cord, the sensory function ascends using the posterior columns of the spinal cord.
By stimulation of peripheral nerves such at the posterior tibial nerve at the ankle, and the median nerve of the wrist, we can evoke an afferent potential that travels up via the peripheral nerve to the spinal cord, to the thalamus, and finally reaching the primary somatosensory cortex of the brain. We can record and analyse the signal and infer the normal function of the sensory pathway. Should changes to this signal be observed, we can infer a cause and provide immediate intervention to predict or prevent new neurological injuries from occurring.
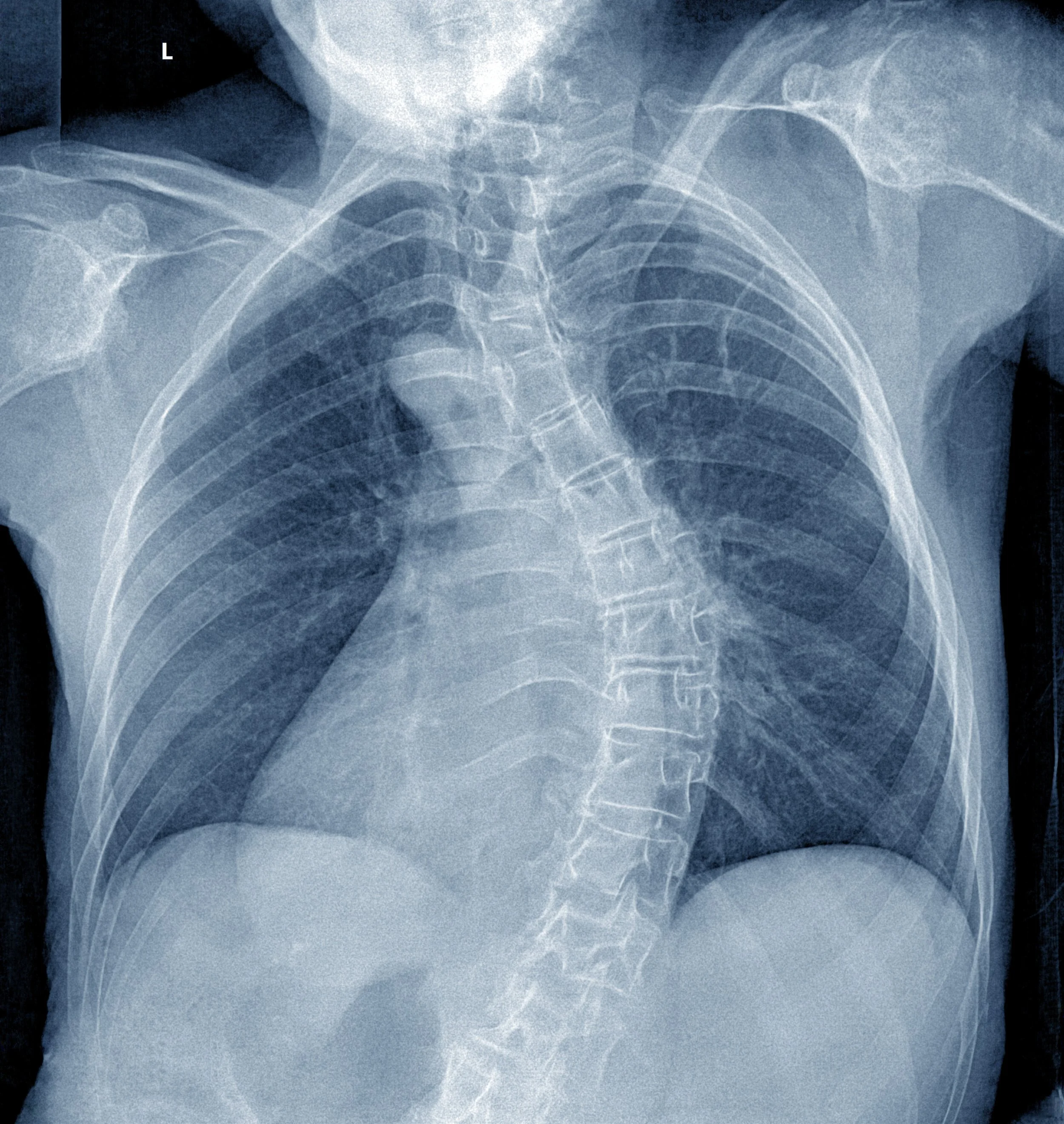
Image: Posterior Spinal Fusion for Scoliosis, is a major surgery that involves correction of an abnormal curvature in a spine. During this procedure, the spinal may sometimes not tolerate the structural realignment of the spinal column and cause severe loss of function. IONM is an important tool used during this procedure to assess the viability of correction, and prevent spinal cord damage.
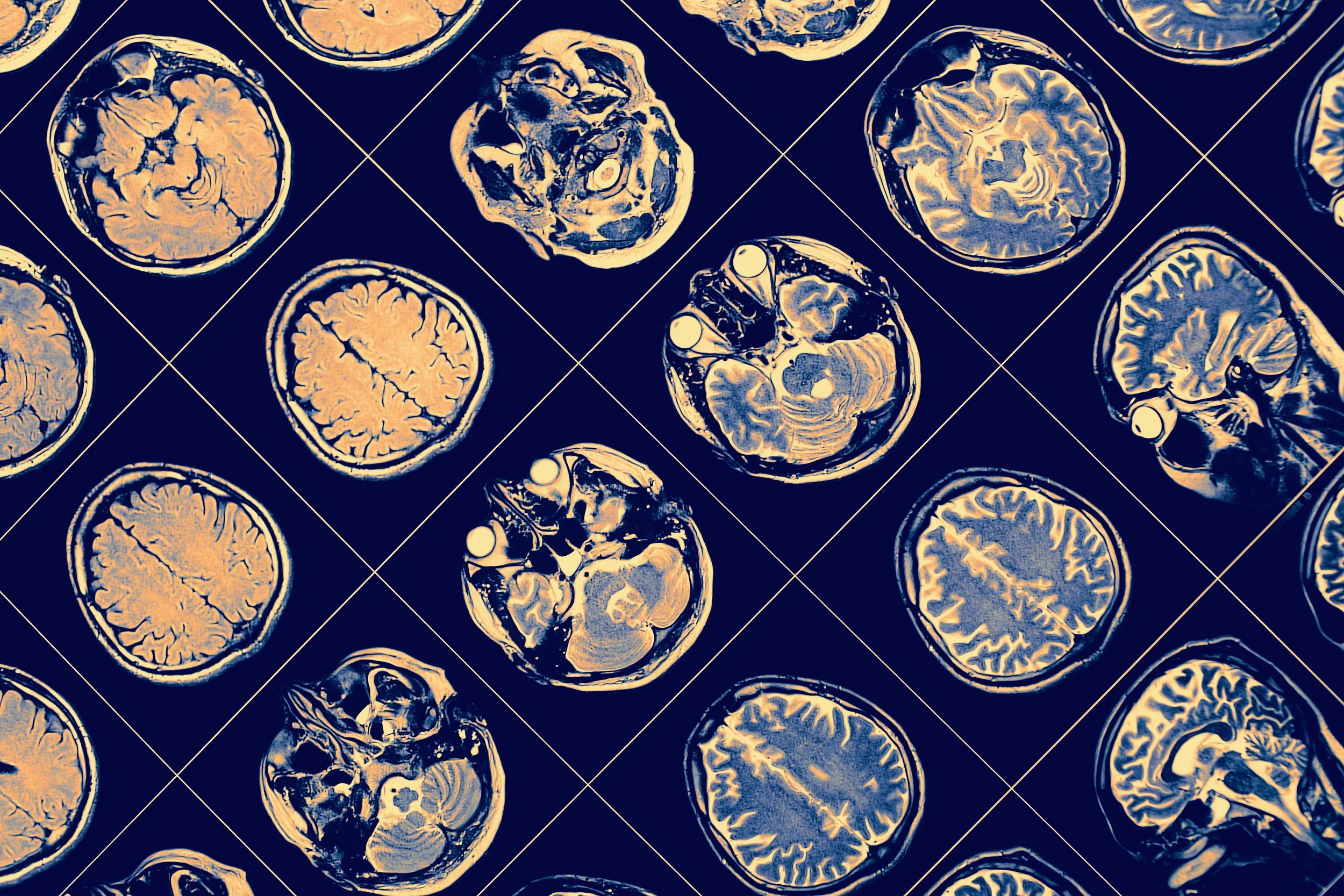
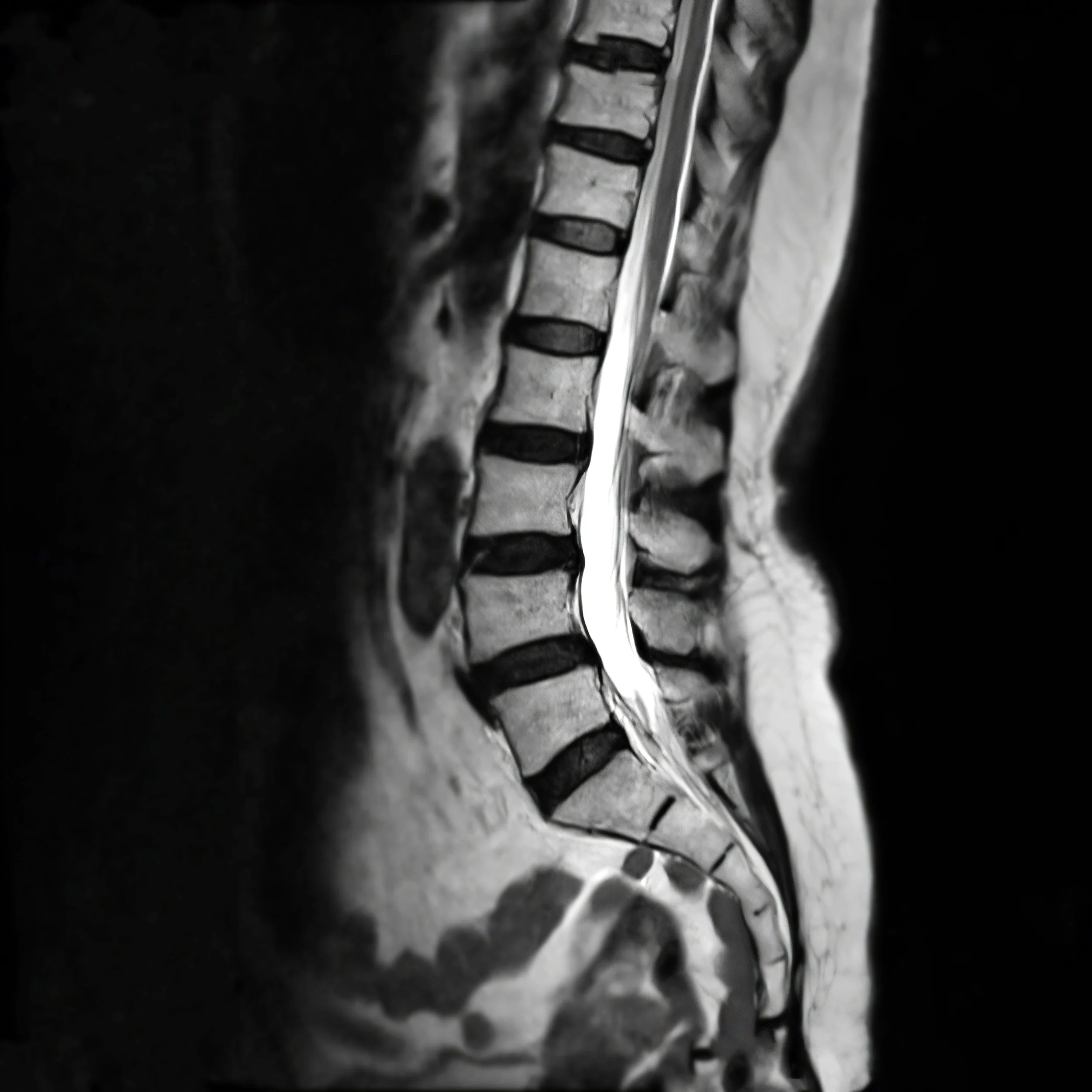
Image: Model (Below) MRI (Above) of the lumbar spine. The lower portion of the back, known as the lumbar and sacral segments of the spine are most prone to injury due to the weight bearing elements for the rest of the upper body. Herniation of the discs in between the vertebrae can push into the spinal nerves and cause neural dysfunction including pain, numbness, or regional paralysis.
Procedures that utilised IONM
There are a number of procedures that utilise IONM, as any procedure where there are risks for neurological damage, IONM may prove to be of benefit. The following is a non exhaustive list of procedures.
Scoliosis and Deformity Corrections
Corpectomy
Transpoas Lateral Lumbar Interbody Fusion
PLIF, TLIF, OLIF, ALIF
ACDF, PCDFs
Intramedullary Spinal Cord Tumour
Extramedullary Spinal Cord Tumours
Spinal Cord Detethering
Thoracoabdominal Aortic Aneurysm
Supratentorial Tumour Resections
Brainstem Tumour Resections
Microvascular Decompressions
Arterial-Venous Malformations
Chiari Malformations
Peripheral Nerve Lesion Resections and Evaluations